25 Oct The phenomenon of MIXED pain syndrome in clinical practice
Mixed pain phenomenon in chronic pain
Chronic pain has been shown to be the result of NEUROPATHIC as well as NOCICEPTIVE pain mechanisms and has therefore been classified as a MIXED pain syndrome (Carlo Luca Romanò,et al).
- Nonspecific nociceptive pain is the result of an inflammatory response to tissue injury
- Neuropathic pain describes cutaneous projected pain arising from the lumbar spine and/or nerve roots (radicular pain or radiculopathy) (Carlo Luca Romanò,et al)
Corollary
- Chronic pain = NEUROPATHIC + NOCICEPTIVE pain mechanisms
- The multifactorial nature of chronic pain such as low back pain has often been underrecognized and undertreated (Carlo Luca Romanò,et al)
Prevalence of neuropathic component in different types of painful disorders
Arthritis
- 22% of OA patients have neuropathic pain (Gore M,et al)
- One-third of Indian patients with RA have evidence of neuropathy (Nadkar MY,et al)
Low back pain
- 41% of the chronic low back pain patients had neuropathic pain and 59% had nociceptive pain (Hassan AE,et al)
Pain of varied etiology in the general population
- 1.5% of the general population has neuropathic pain of varied etiology (Taylor RS,et al
Alerts and Recommendations
Alert -1
Cochrane database evidence from 65 trials
Patients suffering from chronic pain of neuropathic origin following FBSS often fail to obtain adequate relief with conventional therapies (eg, medication, nondrug therapies) and suffer greater pain and lower HRQoL compared with patients with other chronic pain conditions (Roelofs PD,et al).
Recommendation-1
FBSS patients may require alternative and possibly more (cost-) effective treatments, which should be considered earlier in their therapeutic management (Thomson S,et al)
Alert -2
Local injections of steroids are required after failure of analgesics and NSAIDs, in patients with sciatica and chronic back pain (Rozenberg S).
Recommendation-2
- Pain Society/American College of Physicians clinical practice guideline.
- There is fair evidence that tramadol (for radiculopathy) is effective for pain relief. There is good evidence that systemic corticosteroids are ineffective ( Chou R,et al).
- The European League Against Rheumatism (EULAR) recognizes that paracetamol HAS a more significant role to play in the management of chronic pain.
- The American Pain Society suggests that tramadol can be used in combination with paracetamol or NSAIDs, for therapy at any stage during the treatment of a patient with osteoarthritis. Stephan A
In the long-term care of the elderly, the American Medical Directors Association says that tramadol is a first line pharmacological treatment for chronic pain, together with paracetamol, NSAIDs, and COX-2 inhibitors Stephan A
Corollary
Successful treatment of chronic pain depends on identification of the involved mechanism and use of appropriate therapeutic approaches
Role of FEEL AHA in patients with neuropathic component of pain
FEEL AHA is a combination of Tramadol, Paracetamol and Aceclofenac
Tramadol
Ttramadol offers important benefits. Its multi-modal effect results from a dual mode of action, ie, opioid and monoaminergic mechanisms, with efficacy in both nociceptive and neuropathic pain (Schug SA)
Clinical experience of tramadol now extends to more than 5 billion patient treatment days, so the data underlying the latest guidelines are extremely robust (Schug SA,et al).
Paracetamol
Patacetamol reduces thermal hyperalgesia, mechanical and cold allodynia in animal model of neuropathic pain, and might be useful for managing neuropathic pain (Im KS,et al).
Paracetamol also address the nociceptive component of pain (Morlion B).
Aceclofenac
Aceclofenac is a well documented effective and safe NSAID for nociceptive pain
FEEL AHA addresses BOTH the Neuropathic and Nociceptive components of chronic pain
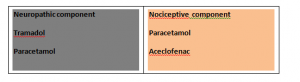
FEEL AHA can be the emerging treatment of choice for MIXED pain observed in CHRONIC pain syndromes
Neuropathic Pain Medicine Brands in India
More known brands:
| REMYLIN D | ERIS LIFESCIENCES* |
| REJUNEX-CD3 | INTAS PHARMA* |
| NUROKIND-D3 | MANKIND |
| NEWBONA ACTIVE | AKUMENTIS HEALTH |
| THE VIBRANIA D | U S V |
| INTAFOL D | INTAS PHARMA* |
| ALL 9-D | AKUMENTIS HEALTH |
| MECONERV-Z | MICRO LABS* |
| COEPREG | KOYE PHARMA |
| MACFOLATE PLUS | MACLEODS PHARMA |
| NURODAY-D3 | WOCKHARDT LTD* |
| UNICOBAL D3 | TORRENT PHARMA* |
| METHYCOBAL-D | WOCKHARDT LTD* |
| DV K PLUS | ALKEM* |
| TRICIUM-PLUS | CORONA REMEDIES |
| ME-D3 | SYSTOPIC |
| JOCARE-OD | D.R.JOHNS LAB |
| HOMO 16 D | SINSAN PHARMA. |
| HOSIT D3 | EMCURE* |
| TRUFOL GYNE | OVERSEAS |
| HOMIN D3 | ICON LIFESCIENCES |
| MAXICAL ACTIVE | MANKIND |
| B-29 DAILY | CORONA REMEDIES |
| ELMECOB-D | TORRENT PHARMA* |
| F029D | AKUMENTIS HEALTH |
References
- Deyo RA. Et al.Spine (Phila Pa 1976). 1996 Dec 15;21(24):2840-9; discussion 2849-50.
- Im KS,et al. Kaohsiung J Med Sci. 2012 May;28(5):251-8. Epub 2012 Feb 22.
- Morlion B. Curr Med Res Opin. 2011 Jan;27(1):11-33. Epub 2010 Nov 18.
- Roelofs PD, et al.Cochrane Database Syst Rev. 2008 Jan 23;(1):CD000396.
- Romanò CL, et al.Pain Res Treat. 2012;2012:154781. Epub 2012 Apr 26.
- Rozenberg S. Rev Prat. 2000 Oct 15;50(16):1789-92.
- Schug SA.et al. Ther Clin Risk Manag. 2007 Oct;3(5):717-23.
- Thomson S, et al.Pain Pract. 2009 May-Jun;9(3):206-15. Epub 2009 Mar 5.




